Eyes are one of the most sensitive organs in the body and tend to get easily irritated due to several different reasons. It is mainly the exposure of the pigmented region of the eye also known as the uveal coat that leads to various disorders such as uveitis or iridocyclitis. Given below is a detailed discussion about iridocyclitis including the causes, symptoms, diagnosis, and treatment of the condition.
Topics Covered
What is Iridocyclitis?
Iridocyclitis is a condition in which the iris and the ciliary body, lying in the middle layer of the eye get inflamed. The condition can be understood in a better light by first learning about the structure of the eye. The iris is the part that lends a specific color to the eye. Therefore, whenever you see blue-grey, green, brown or black eyes, it is the iris that you are seeing. In this center of the iris is the dark circle also known as the pupil. It is the iris that is responsible for controlling the amount of light that enters the posterior chamber of the eye through the pupil. Adjacent to the iris lies a ring of tissues known as the ciliary body. They encircle the eye lens. The ciliary body is responsible for controlling lens shape to adjust vision under different conditions. Apart from that, the ciliary body is also responsible for the secretion of aqueous humor which is a source of nutrient for the eyes.
When both the iris as well as the ciliary body gets inflamed, the condition is known as iridocyclitis. This inflammation is mainly caused due to a direct injury to the eye, an infection, and other related conditions such as arthritis and sometimes for no apparent reason. A person suffering from iridocyclitis will experience an excess of pain and redness in the eye and increased sensitivity to light. If not treated in time, iridocyclitis can also eventually lead to a loss of vision.
Most commonly, iridocyclitis only occurs as a mild condition and only lasts temporarily. The pain and redness usually clear up within a span of a few days or weeks. If the condition has been caused due to other underlying health conditions such as disease and infection, it only goes away after the underlying condition has been treated. It is advisable to opt for treatment as soon as possible in order to prevent severe damage to vision.
Various Types of Iridocyclitis
Depending on its severity and frequency, Iridocyclitis can be divided into the following basic categories:
Acute Iridocyclitis:
Acute Iridocyclitis occurs in a very fast and sudden manner and is accompanied by a large number of symptoms. It does not take very long for acute iridocyclitis to recede. The symptoms start to go away as early as six weeks, and the condition is completely healed in a period of 6 months.
Chronic Iridocyclitis:
Chronic iridocyclitis has a much slower onset as compared to the acute iridocyclitis. It also has a more prolonged existence and lasts for more than three months. It is an asymptomatic condition of the eye and is most often accompanied by systemic disorders such as syphilis, spondylitis, ankylosing, inflammatory bowel disease and Reiter’s syndrome.
Recurrent Iridocyclitis:
This is one of the most common types of iridocyclitis and keeps on coming back even after recovery. With this type of Iridocyclitis, relapsing is quite a common occurrence.
Exogenous Iridocyclitis:
This type of iridocyclitis is caused due to foreign microbes and has an association with uveal injury.
Endogenous Iridocyclitis:
Endogenous Iridocyclitis is caused due to the microbes living inside the body.
Granulomatous Iridocyclitis:
Granulomatous iridocyclitis occurs together with conditions such as keratin deposits or voluminous cellular deposits.
Non-granulomatous Iridocyclitis:
This type of Iridocyclitis is seen together with small cellular deposits in the eye.
Fuchs heterochromic Iridocyclitis:
There is also another type of Iridocyclitis known as the Fuchs Heterochromic Iridocyclitis. In most cases, this is seen to occur unilaterally but may also be bilateral in a few rare cases. Patients suffering from this condition usually do not display any kind of symptoms. Hence, the doctors are required to opt for other methods of investigation for the diagnosis of this condition. The Fuchs Heterochromic Iridocyclitis is most often discovered during the diagnosis of ailments such as heterochromia. Although the exact causes of the condition are not known, it is thought to be a result of neurogenic factors as well as virus infections. Fuchs heterochromic Iridocyclitis is discussed in more detail later in the content.
Different Causes of Iridocyclitis
The uvea or the uveal layer is continuously engaged in functions such as the exchanging of gases and distribution of nutrients in the eyes. Apart from that, the shaded part, that is, the iris and the ciliary body are also involved in the controlling of eye movements and fluid production in the eye. There can be a lot of factors disturbing these normal functions in the eye resulting in iridocyclitis. Some of the common causes triggering the inflammatory response in the iris and the ciliary body are given below.
Problems with the Immune System:
People with underlying problems in the immune system are likely to develop Iridocyclitis. Most of the autoimmune disorders have no specific cause and simply occur due to a faulty autoimmune response, wherein the body attacks its own healthy tissues. Some of the common autoimmune disorders leading up to Iridocyclitis are multiple sclerosis, psoriasis, ankylosing, reactive arthritis, spondylitis, Bechet’s disease, sarcoidosis and juvenile Idiopathic arthritis.
Infections:
Iridocyclitis can also be caused due to infections owing to germs such as bacteria, parasites, viruses, etc. that enter the eyes through the ciliary body or the iris. One such infection is the Herpetic Iridocyclitis caused due to the herpes zoster virus. It affects the pupil resulting in a permanent distortion. The infection may also be accompanied by systemic infections such as tuberculosis, toxoplasmosis, syphilis, and HIV.
Physical Injury:
A direct physical injury to the eyes or a trauma arising out of eye surgery can also lead to Iridocyclitis.
Side effects of Drug Usage:
Sometimes, Iridocyclitis can be caused as a side effect of some drugs. The common drugs that are known to cause Iridocyclitis are Rifabutin, a derivative obtained from Rifampin and quinolones, particularly Moxifloxacin, according to a number of evidence and reports. All types of vaccinations administered to the body are also known to increase the risk for Iridocyclitis.
Exposure to Chemicals:
When the eyes are directly exposed to harsh chemicals, the risk of developing Iridocyclitis is greatly increased. E.g., lachrymators or the chemical used in tear gas for controlling crowd or during warfare may prove to be quite dangerous for the health of the eyes and are known to cause Iridocyclitis in several instances.
Other Conditions:
Sometimes, Iridocyclitis is caused as a result of other underlying conditions in the body. One of the common health conditions leading to Iridocyclitis includes juvenile rheumatoid arthritis. This may also cause the eyes to swell up simultaneously. This is commonly seen in females and in instances where only a few of the joints are affected by the condition. Lymphoma, which is a type of cancer, is also known to cause Iridocyclitis, although it is seen only in rare cases. Sometimes, it is also possible for the exact conditions of Iridocyclitis to remain unidentified.
Symptoms of Iridocyclitis
The common symptoms of Iridocyclitis are
- Redness in the eye
- Lacrimation or water formation in the eyes
- A constriction in the size of the pupils
- Dilation of the ciliary vessels
- Inflammation in the nodules present on the surface of the iris
- Pain accompanied by a burning sensation in the eyes
- Blurry vision
- Developing of photophobia
- Irregularity in the size of the pupil
- Blacking out of the sclera
- Dark floating spots on the surface of the eye that obstruct vision
- Headaches
- Excessive sensitivity when exposed to bright light
- The iris sticking together with the cornea or the lens. This condition is also known as Synechia.
It should be noted that there are different types of Iridocyclitis and the exact symptoms for the different cases would be as given below.
Anterior Chronic Iridocyclitis or Uveitis
Most often, this condition only affects one eye. The symptoms are as follows
- Redness and pain in the eye
- Photophobia
- Blurred vision or a complete loss of vision
- Watery eyes
Intermediate Chronic Iridocyclitis
- Blurredness in vision without any pain
- Appearance of floaters
Posterior Chronic Iridocyclitis
It usually takes a long time for the affected person to develop any symptoms. The common symptoms observed for this condition are floaters, blurry vision without any pain and in some cases, a complete loss of vision.
Iridocyclitis Incidence
Currently, the global data for the prevalence or occurrence of this condition is not known. However, some evidence suggests that every 9 individuals out of 100,000 in the United States are known to get affected by Iridocyclitis each year. Chronic Iridocyclitis is more common in people between the ages of 20 and 59 years. Usually, children are not known to suffer from this condition. However, it can affect people of all age groups and gender. In the Western countries, 50 to 90 % of the cases concerning Iridocyclitis are due to anterior Iridocyclitis while in the Asian countries, anterior Iridocyclitis accounts for about 20 to 50% of the total cases for Iridocyclitis. If neglected, it can also cause a permanent loss of vision. Care should be taken upon contracting iridocyclitis, especially during the cold winter months.
Diagnosing Iridocyclitis
If there is an appearance of any symptom suggestive of Iridocyclitis, it is best to consult an ophthalmologist right away. The diagnosis is made on the basis of the symptoms that are being displayed, the data obtained through the ophthalmic examination as well as the results acquired from the several tests carried out in the laboratories using equipment of extremely high precision. Most often, the doctor starts the diagnosis by questioning the patient about the various conditions that may have been experienced by the patients. He will then conduct an examination using a sit lamp. This process allows the doctors to understand the exact nature of the inflammation and distinguish it from the progression of several other types of inflammation occurring in the body.
Most often, Iridocyclitis is confused for glaucoma. It is the sit lamp test that allows the doctors to differentiate the condition from other types of eye diseases. If the diagnosis is indicative of a toxic, allergic Iridocyclitis or Iridocyclitis in its metastatic form, the case is referred for additional tests by an immunologist, endocrinologist, rheumatologist, otolaryngologist, and more. Most often, the causes of iridocyclitis are exposed without much difficulty. In rare cases, the diagnosis may require special studies such as serology, a process for the determining the presence of immunoglobulins in the tear fluid and a study of the reaction upon the introduction of the antigens into the eyes.
A Dilated Fundus examination may also be done to rule out the possibility of posterior uveitis. The results are positive if there is the presence of white spots throughout the retina together with vasculitis or retinitis. The doctors also look for any underlying causes that might lead to the inflammation. Some of the common underlying causes are tuberculosis, syphilis, herpes simplex virus, herpes zoster virus, toxoplasmosis, ocular candidiasis, and histoplasmosis. The complete diagnosis will include an evaluation through physical examination, diagnostic tests for blood cell count, complete systems review, tests for antinuclear bodies, VDRL, erythrocyte sedimentation rate and Lyme disease titer.
How Long Does the Condition Last?
There are many different types of Iridocyclitis and the recovery period is different for each type. The non-serious types of Iridocyclitis, such as the non-granulomatous Iridoclytis only last for a short while and subside in as little as a few weeks. However, the more severe types of Iridocyclitis may last up to several months and even a year.
Iridocyclitis Treatment
If the treatment processes for Iridocyclitis are conducted in a timely manner, it can prevent the chances of developing any serious complication by a significant degree. Depending on the type of Iridocyclitis, the treatment may last from a few weeks to several months. During the treatment process, care should be taken for the removal of any signs of inflammation along with equal attention to the prevention of scar formation or appearance of joints which can cause many complications in the following period. Hormonal preparations such as the gidrokortizon and prednisolone are commonly used for the purpose of removing inflammations. These may be used natively or in the form of pills. Strong antibiotics are usually recommended in case of festering Iridocyclitis.
Mydriatics may be used for the prophylaxis of joint formation. This is a medical preparation that helps in extending the pupil so as to prevent the union of the lens and iris. In addition to these, non- steroidal anti-inflammatory drugs, ultraviolet irradiation, electrophoresis, laser therapy, warming may also be used for the treatment. If the Iridocyclitis is of the infectious nature or has taken place due to the autoimmune disorders, an application of corticosteroids may be helpful. Doctors may also give prescriptions for antiviral drugs, antihistamines, antiseptics, immunostimulants and cytotoxic agents in the form of intravenous injections or drops.
The treatment of toxoplasmosis/tuberculosis and rheumatic Iridocyclitis are looked over by specialized doctors. This is done in order to ensure a complete treatment of the underlying disease leading up to Iridocyclitis. The same thing is also done if the condition is a result of Syphilis, gonorrhea or diabetes. If the main underlying causes are not addressed, a separate treatment of only the eye will be effective for only a short period and is sure to be followed by a future relapse.
In some cases, surgical processes may also be needed for the treatment of Iridocyclitis. This is mainly done for the removal of any joints appearing in the eye. In extreme cases, this may also be accompanied by the removal of some of the contents of the eyeball. With proper and timely treatment of the condition, the chances of recovery are higher. Complete recovery occurs only in 20 percent of the cases while periodic relapses accompany the remaining 60 percent of the cases. If the condition is chronic, it can eventually lead to a reduction in sight by a significant amount. Therefore, even after the condition has been treated, it is advisable for the patients to go for regular prophylactic examinations from an ophthalmologist. If not treated in time, the condition can advance to cataract, atrophy of the eyeball, gradual decline in the sharpness of sight, entophthalmia and even blindness.
Prognosis of Iridocyclitis
Iridocyclitis is associated with a favorable prognosis. If the patient is given proper treatment, a complete recovery is possible without any complications during the process. However, the condition has high chances of relapsing even after a complete healing. If it is not properly treated in the ensuing period, it can lead to a very poor prognosis.
Complications that may Arise
If left untreated for a sufficiently long period, Iridocyclitis may lead to the following complications.
- Glaucoma
Iridocyclitis often results in chronic open angle glaucoma. This is seen to occur in upto 59 percent of the cases. The mechanisms for glaucoma include neovascularization of the angle and the iris stroma, trabeculitis, cataract surgery and steroid treatment.
- Cataract
Iridocyclitis often leads to posterior subcapsular cataract. This is known to occur in more than 80 percent of the cases and in most cases, it is already present at the time of initial diagnosis. Most commonly, they form during the setting of corticosteroid therapy.
- IOL implementation and cataract extraction may also lead to glaucoma in 3 to 35 percent of the cases.
- Surgery may also lead to cystoid vitreous opacification or macular edema of the protein deposits, and the fluid collects under the macula causing it to thicken and swell
- 12 to 50 % of the cases are associated with vitreous debris leading to symptomatic floaters
- Abnormality in the blood vessels may lead to postoperative hyphema
- Band keratopathy, which is a disease affecting the cornea and arising due to the calcium deposit on the central cornea
- Permanent loss of vision
Preventing Iridocyclitis
It is common for iridocyclitis to keep on relapsing. Therefore, it is considered best to consult an ophthalmologist on the earliest signs or symptoms. Some of the ways in which Iridocyclitis can be prevented include
- Taking strict measures for the prevention of viral and infectious diseases
- Frequent diagnosis of the underlying causes
- Immediately consulting a physician in case of redness in the eye
- Staying away from eye injuries
- Preventing hypothermia
- Taking steps to strengthen immunity
Since Iridocyclitis can naturally arise out of other conditions in the body, care should be taken especially during the colder months. Self-treatment can only be helpful to a very small degree, and it is best to get help from a specialist. Timely treatment is known to increase the chances of a complete recovery without any chances relapsing or other heavy complications.
Iridocyclitis Problem in Children
If Iridocyclitis is seen in children, it is usually in those who have been diagnosed with rheumatoid arthritis. When it occurs in children, the anterior portion of the uvea becomes inflamed and may even lead to a scarring of the pupils. It is also known to have affected the focusing capability of the eye in several different instances. Therefore, the patient is apt to suffer from inflammation in the tissues, joints, and eyes accompanied by a swelling. If there is any presence of the antinuclear bodies, the condition may even escalate to Juvenile Arthritis.
Understanding Fuchs Heterochromic Iridocyclitis
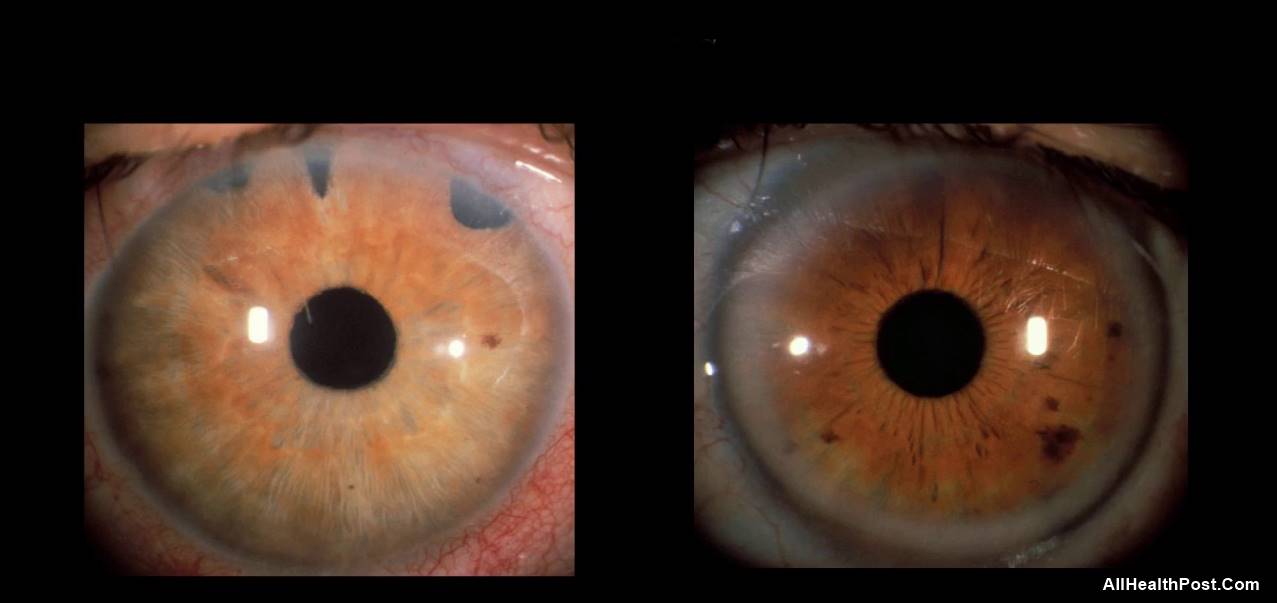
The Fuchs Heterochromic Iridocyclitis was first described in 1906 by Fuchs and hence the name. It is also known as Fuchs Uveitis syndrome, Fuchs heterochromic uveitis or simply FHI. It is a unilateral Iridocyclitis of chronic nature and is most often accompanied by Iris heterochromia. Fuchs proposed that some unknown processes induced a development of an abnormal type of pigment in the uvea. This occurred together with a constant low-grade inflammation. He noticed that if left ignored for a long period, it led to other complications such as secondary glaucoma and iris atrophy.
FHI usually occurs in young adults having lighter colored eyes. It is accompanied by very few ocular symptoms and is not accompanied by any pain or redness in the miosis or the external part of the eye. FHI is also not associated with any of the systemic diseases. Gradual progression of the disease can lead to conditions such as glaucoma, cataract formation, and vitreous cellular infiltrates. Although it is commonly known to occur as unilateral disease, around 7 to 10 % of the cases have been associated with bilateral disease.
Like most other diseases, the characteristics defining FHI have increased with time. Some of the common characteristics accompanying FHI include reversed heterochromia, the absence of heterochromia and peripheral choroiditis with a small focus. FHI is said to be a diagnosis of exclusion, meaning that if the person who is being diagnosed does not appear positive for other types of infectious and non-infectious uveitis, the condition is characterized as Fuchs Heterochromic Iridocyclitis.
Fuchs heterochromic Iridocyclitis may also occur together with idiopathic non-granulomatous uveitis. It occurs in a very subtle manner and is recurrent. FHI is common to appear in females of young ages. The condition is mild, and common complaints include blurred vision. If the symptomatic exacerbation of uveitis is seen, topical corticosteroids may be used for the treatment. Although cycloplegics also tend to be effective, they are used only in a few cases.
Iridocyclitis vs. Uveitis
While Iridocyclitis refers to the inflammation of the ciliary body and the iris, Uveitis refers to the inflammation of the Uvea. In case of the uvea, the inflammation may also spread to other parts including the optic nerves, vitreous humor, sclera, retina and the iris.
Iridocyclitis Vs. Iritis
Both Iridocyclitis and Iritis are integral to the larger term Uveitis. Iritis is the term used for the sub category of anterior uveitis while iridocyclitis is the term used for intermediate Uveitis.
Conclusion
Although Iridocyclitis is not a fatal condition, it can cause quite a lot of pain and discomfort when it occurs. Therefore, it is best recommended to get the treatment as early as possible. It is also common for Iridocyclitis to be mistaken for other eye diseases such as glaucoma or conjunctivitis. Therefore, it is best to go for a proper diagnosis under an experienced ophthalmologist.




